For some time c.1700 and earlier the term "Choler", from Greek Khole, Latin Kholera = bile, anger, LME OED, was applied to any of various conditions characterised by violent diarrhoea and vomiting, including "summer diarrhoea", "summer choler", and cholera morbus. A chicken cholera or "fowl cholera" was also recognised, as was a frequent condition of young children, "choler infantum".
A "cholera belt" of silk or flannel was a waistband — perhaps containing specified herbs, and with a priest's incantation spoken over it to make it a talisman — worn as a sympathetic/magical aid/charm and preventative, before the arrival of rational-empirical modes of thinking..
By the nineteenth-century the terms "Asiatic" and "genuine" cholera had become the commonly accepted designations, at least among the wider educated, and these flourished alongside keenly descriptive medical phrases such as "the malignant diarrhoea" and "rice water stools". As noted by the later German bacteriologist Carl Fraenkel (1887: 259) however, "Science sought for the cause and mode of origin of the mysterious disease in vain; opinions and views sprang up in abundance, but none offered a satisfactory explanation". A decade later the authoritative British bacteriologists Professors Robert Muir & James Ritchie were equally sceptical of earlier workers, asserting that "previously to 1883 practically nothing of value was known regarding the nature of the virus [= disease substance, from Latin for slimy, poison, E18 OED] of cholera. In that year [Robert] Koch was sent to Egypt, where the disease had broken out" (1897: 446).
To the Victorian and Western consciousness in Europe and the Americas, the definitive emergence of the fearful epidemic disease-contagion soon to be known simply as Cholera, may be conveniently dated from 1816-26 and the First Bengal Cholera Pandemic, also noted by contemporary physicians and hygienist-epidemiologists as Bengal Cholera, Asiatic Cholera and "Agide cholera", or "the Eastern Cholera", which by c.1830 had spread to Russia, Eastern Europe, Germany, and Britain, with the inevitable transmission via the shipping-lanes to the eastern seaboard of the United States and beyond by 1832-33.
Medical men directly involved in the Bengal disaster included Sir James Annesley (1774-1847), surgeon in India, Member of the College of Surgeons, and Examiner of Medical Reports of the Honourable East India Company. Annesley (1825), in a wholly pre-bacteriological medical environment, produced probably the first major publication on the "Epidemic Cholera of the East". His major clinical and therapeutic recommendation to his Madras authorities was the medicinal application of calomel (Mercuric chloride), a sweet-tasting but toxic heavy metal salt, which had been recommended and employed by the American physician-chemist and inspirational teacher of medicine Benjamin Rush (1746-1813) during the 1793 outbreak of Yellow Fever in Philadelphia. Annesley's work was quickly taken up and published in cholera-afflicted Germany a few years later. Along with the intensive "bleeding" of leech-therapy, it should probably be viewed as partly derived from the concepts of the so-called heroic rather than of rational medicine.
David Carruthers (1830), another British and East India Company physician, worked with Annesley in Madras during the Bengal Cholera Epidemic. The subsequent study of Carruthers was a comparative work, and covered not only the Bengal outbreak but also the subsequent and related European Pandemic of 1829 onwards. His data indicated that some ten thousand British troops had perished by the disease in India, along with "hundreds of thousands" of native Indians. Follow-up studies were not lacking, from both sides of the Atlantic, for example Bell & Condie (1832), Thomson (1848), Jones (1849), Cox (1849), Stevens (1853).
William Marsden (1796-1867), an English surgeon, founded in London the Royal Free Hospital in 1828 and the Royal Marsden Hospital in 1851. His major report, Marsden (1865), covered five cholera outbreaks in England between 1832 and 1854. The following two decades would see the new and essential science and practice of bacteriology began to pass from its infancy to a more thorough-going discipline of sampling, culturing and histological-staining and identification. It would also see a plethora of continuing "pre-bacteriological" studies of the Asiatic-Eastern Epidemic Cholera, with Histories and Summaries of each new and cumulative outbreak from India and across the western world. Sadly, the diligence of the many medical authors, Local and Government , and committees would provide little or no advance in the correct understanding of the actual etiology and disease transmission-pathway of the deadly disease. Hygienists therefore remained hampered in the search for successful prevention, and the medical profession found itself reluctantly pressed towards "heroic" and largely desperate measures, such as purging and bleeding patients already prostrate with an intestinal-fecal disease and burning soiled clothing and bedding when the local water-supply was invisibly contaminated.
Post-1883 and the Discovery of the Komma Bacillus of Koch.
In 1883 a fresh outbreak of Cholera in India persuaded the Imperial Government in Berlin to send an Imperial Commission, led by Koch together with a number of his colleagues and assistants, to study and master the feared disease once and for all. A First Cholera Conference was convened in Berlin in 1884, to which Koch famously delivered his definitive results. Also in 1884, a cholera epidemic at Naples led the Bavarian government to similarly send the Munich bacteriologist and paediatric epidemiologist Emmerich to identify the cause or causes. Emmerich's bacillus neopolitanus was proposed - perhaps in part politically - both partly to confirm and partly to contradict the prior findings of Koch and the Berlin group. Other competing candidate-bacteria were at that time also proposed as the causative agent of cholera or similar diseases: Finkler & Prior's Spirillum, Deneke's Spirillum, Miller's Spirillum, Heider's vibrio danubicus from canal water, and so on.
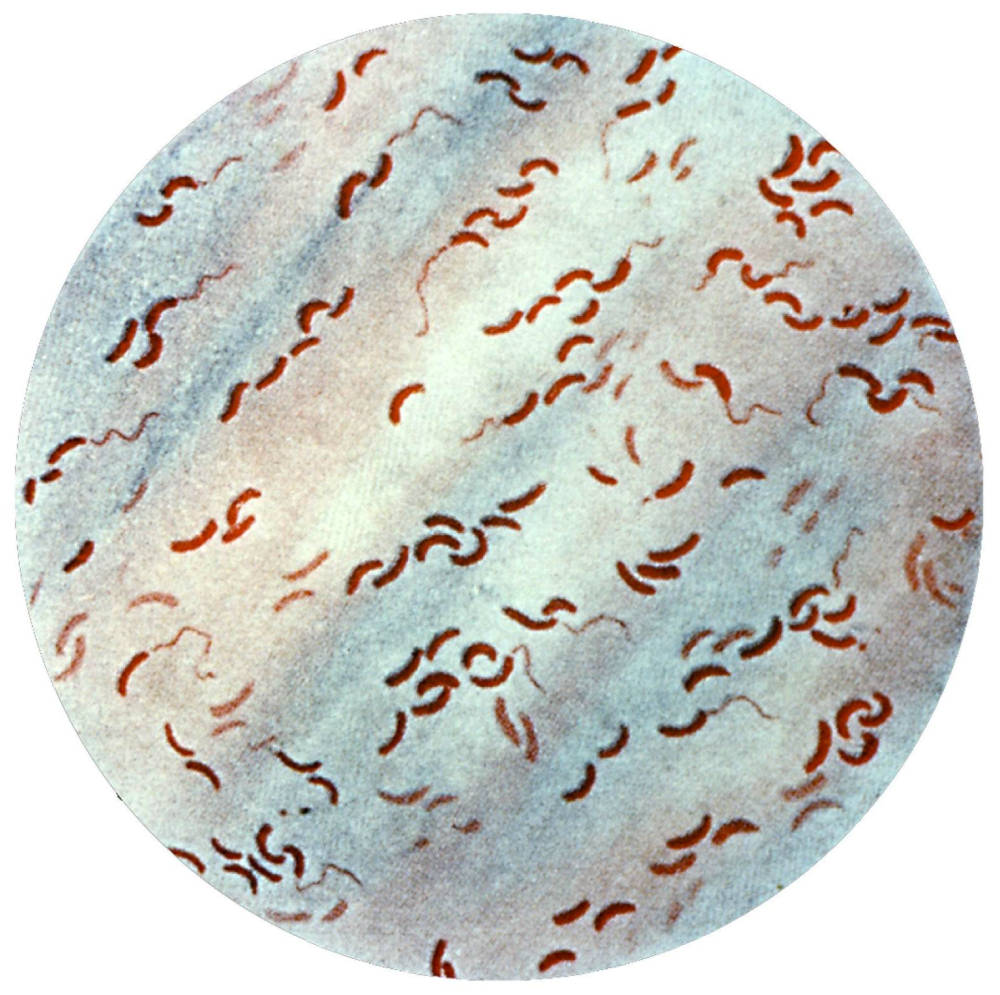
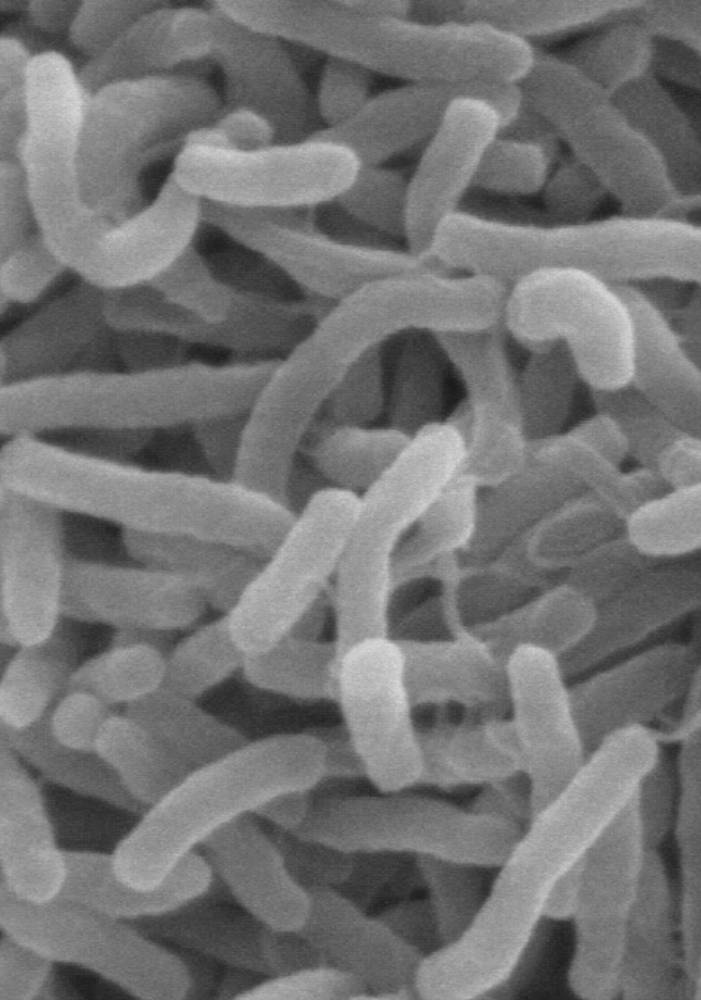
Left: The Komma Bacillus of Cholera. Courtesy of Pixnio. Right: Gram-stain permits visualization of flagellate bacillus of cholera. Courtesy Wikimedia. [Click on images to enlarge them.]
Koch's Komma bacillus, named after resemblance of its curved shape to the comma of punctuation, was initially seen in its early developmental form, which confirmed the previous description by Italian anatomist and microscopist Pacini (1854). Typically confined to the intestines and profuse fecal wastes, with no migration to other bodily organs such as seen in TB, syphilis, gonorrhoea, anthrax, the small organisms, staining well with methylene blue or carbol-fuchsin, will eventually when cultured develop to show their true form as twisted Spirilla or Vibrios. German workers often preferred the term vibrio cholerae whereas British workers preferentially employed the name "Cholera spirillum" (Fraenkel 1887: 266ff; Muir & Ritchie 1897: Chap. XVIII).
The organisms are extremely motile, with a single whip-like flagellum as tail. It is endemic, especially in the Indian sub-continent, though the powers of resistance of the disease organism are not great. The vibrio quickly succumbs to dry conditions, with no spore formation; to heat and steam; to other competing micro-organisms in sewage etc.; and to simple disinfectants such as lime, as demonstrated by Pfuhl. The dramatic and acute onset of the disease was quickly linked to the production of powerful toxins which entered the bloodstream, and numerous workers raced to find anti-sera/antitoxins, including Pfeiffer with Koch in Germany; Elie Metchnikoff and Emile Roux in France; and Macfadyen, Klein and others in Britain. Haffkine undertook a large-scale inoculation exercise in India in 1894, employing attenuated cholera organisms which had been weakened by various techniques. Cholera-carriers were known, though less noted than for other diseases, e.g. with the notorious Typhoid Mary in the U.S. A large number of dedicated bacteriological workers involved themselves in cholera research, including Nikati & Rietsch, Sabolotny, Kolle, Pettenkofer; Dr. Orgel of Hamburg, who died in 1894 after contracting cholera during his experiments with the vibrio; Kraus, Schurupoff, Dunbar, Gotschlich, Ivanoff; Pestana & Bettencourt during an epidemic in Lisbon; Celli & Santori with their Spirillum v. Romanus; Neisser in Berlin, Cunningham (1890) in India, and others. See also MacNamara (1892), Nichols (1909), McLaughlin (1916), Vincent & Muratet (1917).
Related Material
Last modified 19 December 2022